Employers feel immense pressure to control healthcare costs while offering benefits and programs that help employees thrive personally and professionally.
In fact, 85% of employers say surging healthcare prices are their biggest benefits challenge.1
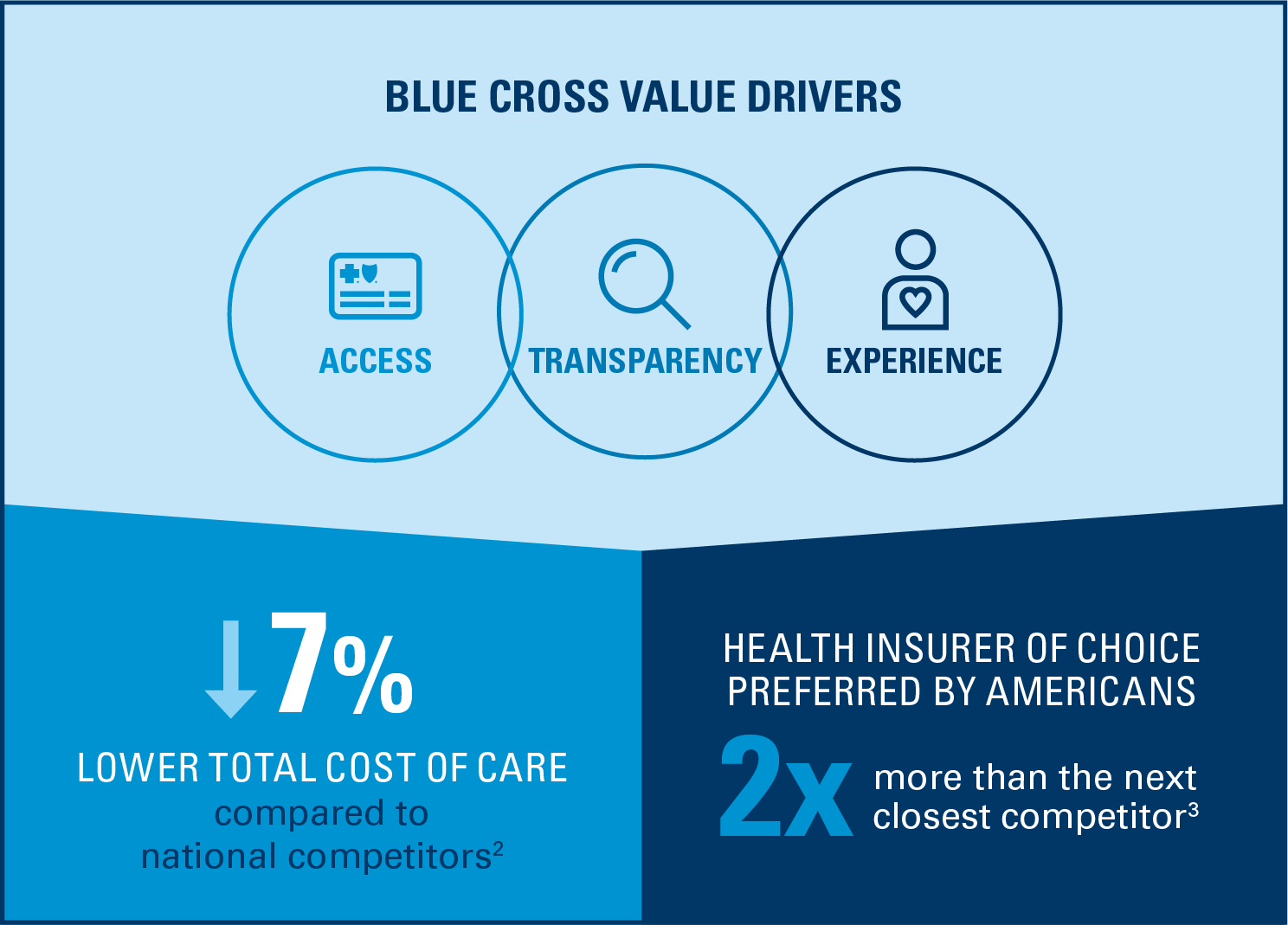
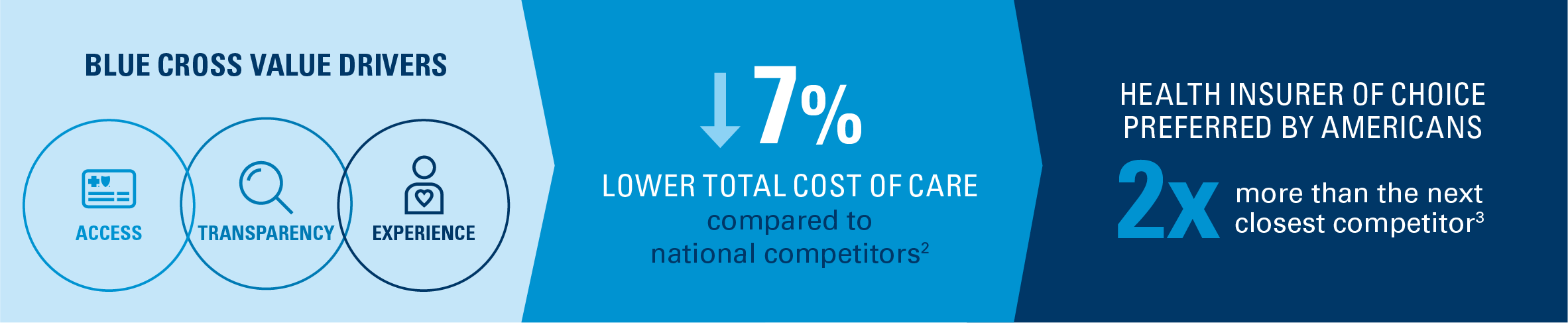
Benefit leaders can count on Blue Cross and Blue Shield of Minnesota. Our trusted operating model is anchored in access, transparency and experience — which delivers 7% lower total cost of care (TCOC) compared to national competitors2 with people preferring Blue Cross two times more than the next closest competitor.3
This means employers that choose Blue Cross achieve real savings on health benefit costs, not just short-term fixes, while helping their employees live their healthiest lives.
Access

Providing more choices makes coverage more affordable
With the industry’s broadest network, Blue Cross members have more options to stay in-network and access quality, cost-effective care — reducing out-of-network expenses for both employees and employers. Included in the Blue Cross network is our behavioral health network, which has grown by 55% since 2019.4
And through value-based care contracts that reward providers for positive health outcomes, we help you and your employees achieve sizeable cost savings for each treatment episode.5
98% of claims paid in network6
The industry's broadest global network offers members more options to access quality, cost-effective care.
20% savings per care episode5
Value-based provider care contracts deliver positive outcomes and bottom-line savings for members and employers.
48-hour commitment
Expanded behavioral healthcare access enables timely treatment for youth — including urgent appointments within 48 hours.
Transparency

Using data to facilitate smarter decisions and expand value
By harnessing the power of AI technology and Blue Cross Blue Shield Axis® Provider Insights, we’re able to provide deeper clarity and savings for employers and members.
Axis Provider Insights is the nation’s largest health data repository and tracks the performance across cost and quality of more than 400,000 individual physicians across 20 specialties, including primary care.7 Applied data results in:
High-performance healthcare
Advocating for employers and members by negotiating a strategic, robust network of care
Tailored messaging that drives member engagement
Personalizing recommendations designed to close gaps in care before they become more costly
Smarter healthcare decisions
Providing members with transparent cost and quality information to guide them in seeking appropriate care
Experience

Building trust to improve outcomes
Our advanced care management strategy leverages predictive analytics to identify members with complex conditions for outreach and personalized support. This proactive approach helps reduce medical cost trend by up to 19%.8
In addition, our digital navigation solution, Blue Care Advisor,SM encourages members to close care gaps and guides them to high-quality, cost-effective providers.
Combined with award-winning customer service,9 the Blue Cross experience results in high levels of member satisfaction. It’s made Blue Cross America’s most trusted health plan for 16 years in a row.10
19% trend reduction in medical costs8
Predictive analytics determine risk to recommend individualized care plans that have a proven impact on improving outcomes while lowering costs.
104k care gaps closed11
Users followed recommendations through Blue Care Advisor to close care gaps for the first time in at least two years.
2x as likely to get preventive exams11
Compared to those who are not registered, Blue Care Advisor users are more likely to take charge of their health with preventive care.
Optimize plan value with Blue Cross
Move beyond short-term fixes toward cost-effective, long-term quality with a trusted operating model built on access, transparency and experience.
Check out our TCOC infographic for a snapshot of our trusted approach — and download our white paper for a deeper look at how Blue Cross is delivering value in healthcare. Or connect with a Blue Cross representative to learn more.
1 2025 Lockton National Benefits Survey, April 2025.
2 Singleton A, Tilley C, Rachlin S. “Milliman Analysis of Total Cost of Care Benchmarks,” March 2025.
3 Market Insights, Blue Cross Brand Strength Measure Survey, Blue Cross Blue Shield Association, 2024.
4 Blue Cross Blue Shield Association, “Access to Mental Health Support Is Growing as Blues Add Providers,” October 2023.
5 Blue Cross Blue Shield Association, COE results and registry data, BDC/BDC+ eligible providers vs. relevant comparison group. Results based on most recent designation cycle for each specialty. Savings based on BDC/BDC+ total episode cost.
6 Leading consulting firm discount benchmarking report, CY2021, BlueCard PPO.
7 Blue Cross Blue Shield Association internal data, March 2025.
8 Blue Cross and Blue Shield of Minnesota internal data, 2024.
9 Customer service accolades, including Plant-A Insights Group, LLC, USA Today America’s Best Customer Service 2025, multiple online access surveys, U.S. Census 2024, ZoomInfo Technologies LLC, Etailinsights, Onclusive and Critical Mention.
10 “Is a name you can trust” (phone interviews conducted 2010 – 2013) or “Is a company I can trust” (online interviews conducted 2014 – 2025), Brand Strength Measure Survey, Blue Cross Blue Shield Association.
11 Blue Care Advisor internal data, 2024.