It’s important that you see doctors in your health plan’s provider network if you want to get the highest level of coverage from your plan.
Find a Doctor FAQs
While our networks are very large, specific doctors and other health care providers listed in this tool may not be in your health plan’s network. It's important to log in and search the right network to make sure you’re seeing doctors, clinics and hospitals covered at the highest level by your health plan. If you visit providers who are not in your network, your out-of-pocket costs are likely to be much higher.
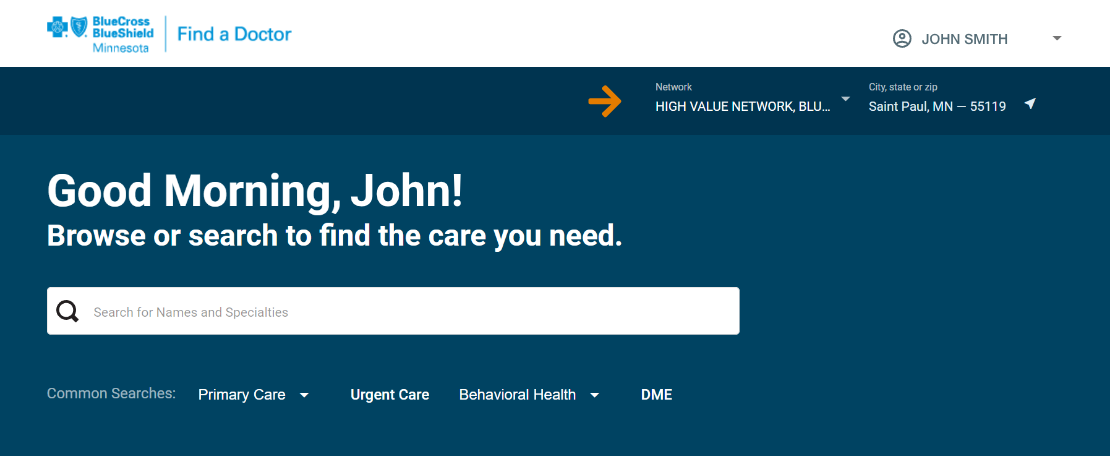
The best way to make sure you’re searching the right network is by logging in. By providing the info on your ID card, we will know your network and only show results from your network after you log in. You can also:
- Refer to your plan materials, such as your Summary Plan Description, plan contract or sales materials, for the name of your provider network.
- Call customer service at the number on the back of your member ID card.
How can I find more health care providers?
If you're seeing limited results, try adjusting your search:
- Use fewer or more general words
- Adjust the location information or miles
- Search by specialty (ex. Pediatrician)
- Try using a city and state if the city has more than one ZIP code
- If you've narrowed your search by customizing your results (for example, by selecting a gender), undo the customization
- Try following a guided category search
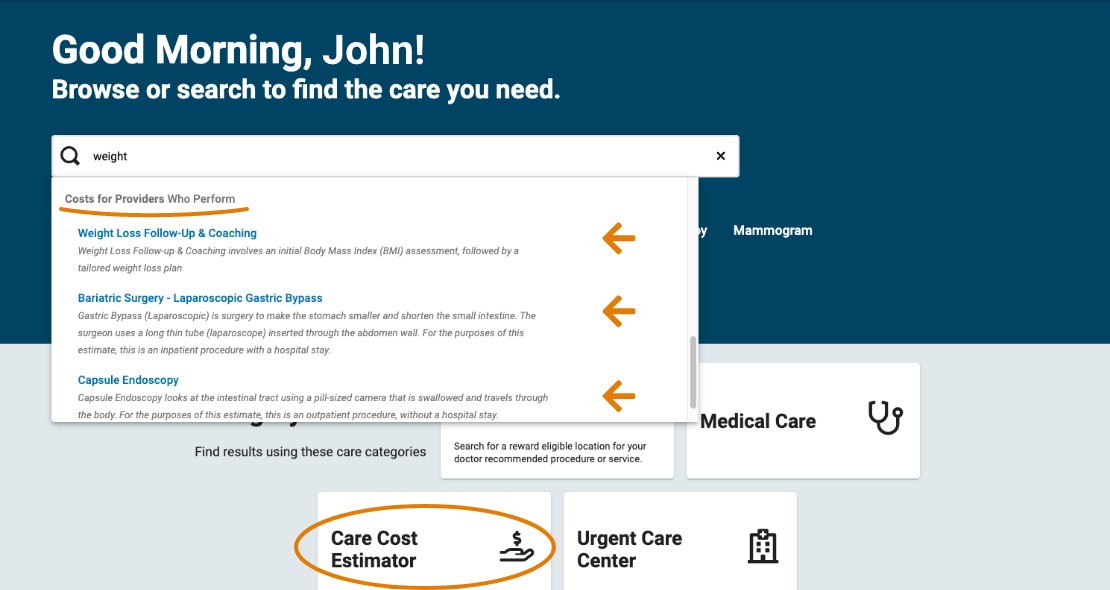
How do I look up costs for a procedure?
Those with employer-provided or individual and family plans can use this tool to see estimated costs for 1,700+ procedures and services. This does not currently apply to Medicare members.
Step 1: Sign in or register for a member website or member app account
Step 2: Navigate to Find a Doctor
Step 3: Enter the procedure name into the "Find a doctor" search field
Step 4: Wait a second for the drop-down list to appear
Step 5: Select the procedure you want
Step 6: Review overall cost estimates and select a provider to see more detail
You can also choose "Care Cost Estimator" and follow a guided path to procedure with cost estimates.
What do the search criteria filters mean and who supplies the info?
Most Find a Doctor information is provided by each health care provider or facility and updated as needed through the contracting process with Blue Cross.
Specialty – This is the medical specialty for which the health care practitioner is credentialed to provide medical services to our members. Specialty qualifications are verified through the appropriate specialty board or residency training program.
Hospital affiliations – These are hospitals in the health plan network where the provider has admitting or attending privileges. Please note that if a hospital does not contract with the health plan, it is not listed in this directory.
Medical group affiliations – A listing of all medical groups with which the health care practitioner is associated (when applicable). If the practitioner does not provide this information, it is not included in this directory.
Board certification – When a doctor successfully completes a program and testing for a particular specialty, they achieve board certification. Board certification shows a physician's expertise in a particular specialty and/or subspecialty of medical practice. A physician's board certification status, including expiration date (if applicable), is verified directly with the American Board of Medical Specialties (ABMS).
For specialties in which the physician has achieved certification, the specialty is listed as "Board Certified." Board certification status is updated with the ABMS when it expires, but there may be some situations when data is not current due to the timing of website updates.
For a majority of physicians, you can verify a doctor's current board certification status through the American Board of Medical Specialties. Board certification is current if the doctor is listed on the ABMS website as "General" or "Specialty" certified.
Acceptance of new patients – Indicates whether or not the provider is currently accepting new patients. This information is updated as reported by the practitioner.
Languages spoken by health care provider or clinical staff – Indicates any languages (other than English) spoken by the practitioner or clinical staff in the office. This information is updated periodically through provider network outreach.
Location – The address of the practitioner office or hospital. It is updated as reported by the practitioner or hospital upon relocation.
Hospital accreditation – Accreditation is a voluntary process that evaluates whether a hospital meets designated standards for health and safety. A hospital's accreditation status is verified directly with the Joint Commission.
Although accreditation is verified every three years, any changes in status reported by the hospital are updated in this directory as quickly as possible. The frequency of updates may vary for providers outside of Minnesota.
What is a Blue Distinction Center (BDC)?
Blue Distinction Centers are hospitals recognized for their expertise in delivering specialty care.
Can I get a printed list of all doctors, hospitals and clinics in my network?
Our networks contain many doctors, clinics and hospitals. Because doctors enter and leave our networks, a printed list of providers would be very large and quickly become outdated. To print the results of a search, use the "Save as PDF" link at the bottom of the search results page.
How do you get the information about the health care providers?
The health care providers (such as doctors) and hospitals we contract with give us this information in the credentialing process. Credentialing is checking the accuracy of the reported qualifications of licensed health professionals or organizations. It also involves reviewing a provider’s background, such as education and training, to make sure they meet certain professional requirements.
Credentialing happens when a health care provider or hospital first applies to provide services to members in the network. For Minnesota providers, recredentialing happens at least every three years after that. This may vary in other states.
We also receive information on our providers in the contracting process. Contracting is when a health care provider or hospital agrees to provide services to our members and is done every three years.
How do you verify the information?
The information is verified through the credentialing and/or contracting process referenced above.
How often do you verify the information?
The information is verified at credentialing and/or contracting and every three years at recredentialing for providers in Minnesota. This may vary for providers in other locations. Where noted in the next question, it is updated and verified at additional times.
Be sure your doctor and service are covered
Blue Cross and Blue Shield licensees have made reasonable efforts to ensure that the list of providers displayed is up-to-date and accurate. Please call the provider before making an appointment to verify that the provider continues to be part of the network. Members should refer to their benefit contract or contact their plan's customer service department to determine if the provider type is covered. Members should also ask customer service if the treatment requested from a network provider is covered.
MNsure Network Design Criteria for Physicians and Hospitals
All MNsure plan networks consist of participating primary care physicians and a full range of specialists. When developing the network, consideration is made of the location of clinicians and hospitals in relation to where members live. Our aim is for all members to have access within a reasonable distance to all types of clinicians and hospitals. The decisions about whether or not to add a clinician or hospital to the network is based on their ability to provide care to members and does not use quality, member experience or cost related measures.